
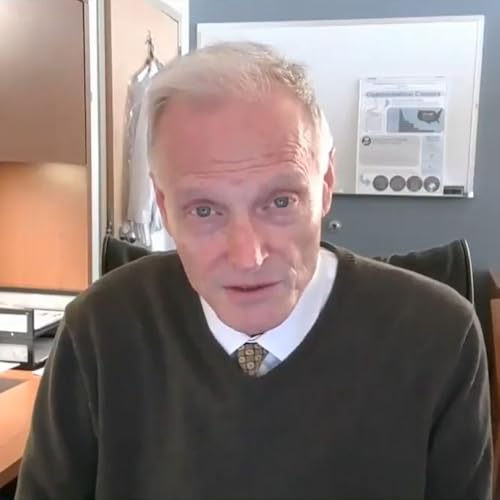
Oncology Unscripted With John Marshall
Artikel konnten nicht hinzugefügt werden
Leider können wir den Artikel nicht hinzufügen, da Ihr Warenkorb bereits seine Kapazität erreicht hat.
Der Titel konnte nicht zum Warenkorb hinzugefügt werden.
Bitte versuchen Sie es später noch einmal
Der Titel konnte nicht zum Merkzettel hinzugefügt werden.
Bitte versuchen Sie es später noch einmal
„Von Wunschzettel entfernen“ fehlgeschlagen.
Bitte versuchen Sie es später noch einmal
„Podcast folgen“ fehlgeschlagen
„Podcast nicht mehr folgen“ fehlgeschlagen
-
Gesprochen von:
-
Von:
-
John Marshall
Über diesen Titel
Folgen
-
 34 Min.
34 Min.Artikel konnten nicht hinzugefügt werden
Leider können wir den Artikel nicht hinzufügen, da Ihr Warenkorb bereits seine Kapazität erreicht hat.Der Titel konnte nicht zum Warenkorb hinzugefügt werden.
Bitte versuchen Sie es später noch einmalDer Titel konnte nicht zum Merkzettel hinzugefügt werden.
Bitte versuchen Sie es später noch einmal„Von Wunschzettel entfernen“ fehlgeschlagen.
Bitte versuchen Sie es später noch einmal„Podcast folgen“ fehlgeschlagen
„Podcast nicht mehr folgen“ fehlgeschlagen
-
 22 Min.
22 Min.Artikel konnten nicht hinzugefügt werden
Leider können wir den Artikel nicht hinzufügen, da Ihr Warenkorb bereits seine Kapazität erreicht hat.Der Titel konnte nicht zum Warenkorb hinzugefügt werden.
Bitte versuchen Sie es später noch einmalDer Titel konnte nicht zum Merkzettel hinzugefügt werden.
Bitte versuchen Sie es später noch einmal„Von Wunschzettel entfernen“ fehlgeschlagen.
Bitte versuchen Sie es später noch einmal„Podcast folgen“ fehlgeschlagen
„Podcast nicht mehr folgen“ fehlgeschlagen
-
 24 Min.
24 Min.Artikel konnten nicht hinzugefügt werden
Leider können wir den Artikel nicht hinzufügen, da Ihr Warenkorb bereits seine Kapazität erreicht hat.Der Titel konnte nicht zum Warenkorb hinzugefügt werden.
Bitte versuchen Sie es später noch einmalDer Titel konnte nicht zum Merkzettel hinzugefügt werden.
Bitte versuchen Sie es später noch einmal„Von Wunschzettel entfernen“ fehlgeschlagen.
Bitte versuchen Sie es später noch einmal„Podcast folgen“ fehlgeschlagen
„Podcast nicht mehr folgen“ fehlgeschlagen
Noch keine Rezensionen vorhanden



